So many diabetes patients—especially those diagnosed with Type 2 diabetes—believe that a little pill takes care of everything. In all fairness, the recent rash of TV commercials featuring happy people using miniaturized, painless, at-home blood sugar meters seems to put diabetes one notch beneath the sniffles. So it’s no great surprise that many newly diagnosed diabetes patients are shocked to learn that the disease can affect their whole body so profoundly. There is, however, much a diabetes patient can to do promote a healthier life and prevent complications—from shedding excess weight to staying active and most important of all, understanding that properly managing diabetes is a lifelong commitment.
KNOWLEDGE IS POWER
To help patients fully grasp what it takes to successfully manage diabetes, UHS endocrinologists, nurse practitioners, diabetes educators, registered nurses and registered dietitians are available for ongoing, compassionate support and education.
Brenda Kosydar, RN, BSN, CDE, diabetes nurse educator at the Diabetes and Endocrinology Center, often begins class with a statistic—a wakeup call—because initial confusion about diabetes is common. “Many patients say, ‘I don’t know why I’m here! All I have is a little sugar.’ I respond by explaining how they were diagnosed and what their labs mean, particularly the HbA1C or hemoglobin A1C test. One of the statistics we share is that 80 percent of people diagnosed with diabetes will die from cardiovascular disease.”
“I also say it doesn’t have to be that way if you manage your diabetes, whether Type 1 or Type 2,” she continues. “And eating healthy and exercising is the answer. Then the light bulb goes on. Suddenly everyone’s interested in meal planning, exercise programs and knowing what their hemoglobin A1C test results mean.”
TEAM TEACHING
Understanding diabetes management is an essential step in treating the disease, says Jillene Brathwaite, DO, endocrinologist at UHS Wilson Medical Center. “This is a progressive disease with potential long-term complications. We can often control these complications, but only if the patient works with us, which can be very challenging. We’re usually asking patients to change lifestyle choices that were learned at a young age.”
To strengthen the educational impact, a patient’s communication loop includes every member on the patient’s team. “A patient’s blood glucose report begins with the educator, who advises the patient, but the report is also communicated across the board,” Dr. Brathwaite stresses. “We all know at all times where the patient’s health and diabetes management stands.”
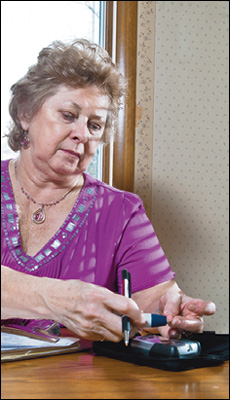
Beverly Cook has better control of her diabetes today.
CONTINUING EDUCATION
Not everyone attending a UHS diabetes class is a newcomer to the disease. Beverly Cook, 68, was diagnosed with Type 1 diabetes in 1962 and was on insulin injections until 2011, when she received an insulin pump. To learn to use the pump, Ms. Cook started working with Ms. Kosydar.
“I download my blood sugar levels from the pump, into the computer, and send the numbers to Brenda,” Ms. Cook explains. “My nurse practitioner reviews the download with the physician and will order a change in the pumping protocol if needed. Brenda will then help me implement the change, and will keep my doctor informed. I have an A-1 team, and we have everything well managed.”
And if all is not being well managed, Ms. Kosydar and her fellow UHS diabetes educators are available for one-to-one consults. “Sometimes we have to regroup and ask the tough questions,” she says. “Did you lose weight? Are you checking your blood sugars at home? Did you start exercising? Fortunately, we have a great team across the UHS system, and everyone’s here to help get that patient back up and managing his or her diabetes.”
TEST TIME
The primary test for diabetes, both Type 1 and Type 2, is a glycated hemoglobin test, often called an A1C. This blood test delivers your average blood sugar level over three months. An A1C level of 6.5 percent or higher is diagnostic of Type 2 diabetes. Another way to diagnose diabetes is with two separate fasting blood sugar tests over 125. An A1C level of 5.7–6.4 or fasting blood sugar levels on two separate occasions of 100–125 can indicate pre-diabetes. If diagnosed with diabetes, this test is typically repeated every three months.
Keeping up with a regular testing schedule can help prevent complications from diabetes. Throughout the year, your doctor will check your blood pressure and run blood and urine tests to assess your cholesterol levels and thyroid, liver and kidney function. It’s also important to have annual diabetic eye exams with an ophthalmologist as well as foot exams with a podiatrist.